2023 Massey TBI Grand Challenge funds 4 research teams
ANN ARBOR - The University of Michigan Max Harry Weil Institute for Critical Care Research and Innovation announced that it has awarded over $500,000 in research funding to four teams through the 2023 Massey Traumatic Brain Injury (TBI) Grand Challenge Wolverine Den. Supported by the Joyce and Don Massey Family Foundation, the event marked the second Grand Challenge Wolverine Den to take place this year, following the Kahn Pediatric Critical Care Grand Challenge in April.
The competing teams’ projects ranged from novel devices to preclinical models, all united with the goal of improving the diagnosis, monitoring and treatment of TBI during the initial “golden hours” after injury. Judging the teams’ presentations were experts from clinical and commercialization backgrounds, including representatives from the United States Department of Defense.
The winning teams will be able to connect with previous Grand Challenge awardees, as well as with field and industry specialists from both Michigan and abroad, at the upcoming Massey TBI Regional Conference in October.
2023 Massey TBI Grand Challenge Funded Projects
Modeling the relationship between automatic optic nerve sheath diameter measurements from computed tomography scans and intracranial pressure in traumatic brain injury patients
PI(s): Erica Stein, MD; Kayvan Najarian, PhD; Emily Wittrup, MS; Craig Williamson, MD
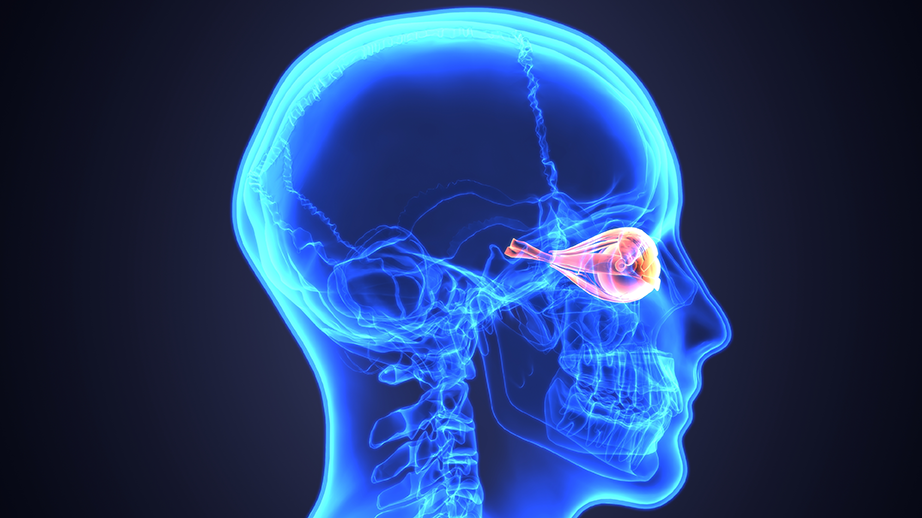
During the golden hours of TBI, obtaining an accurate measure of intracranial pressure (ICP) is critical. The current gold standard measurement for ICP is obtained through invasive intracranial devices, which can be time-consuming to insert and expose the patient to additional risks.
Optic nerve sheath diameter (ONSD) is known to be affected by changes in ICP, with previous studies demonstrating the value of ultrasound-assessed ONSD compared to invasive measurements. There are limitations to this method, however, such as a high degree of variability. Given this, the team will instead explore the use of obtaining ONSD measurements through computed tomography (CT) scans. Because head CT scans are routinely collected for TBI patients, obtaining the ONSD measurement concurrently instead of separately with ultrasound would save critical time in the golden hours of a TBI.
Glycemic variability following traumatic brain injury: utilizing a continuous glucose monitor in the golden hours to improve patient outcomes
PI(s): Katharine Seagly, PhD; Nathan Haas, MD;
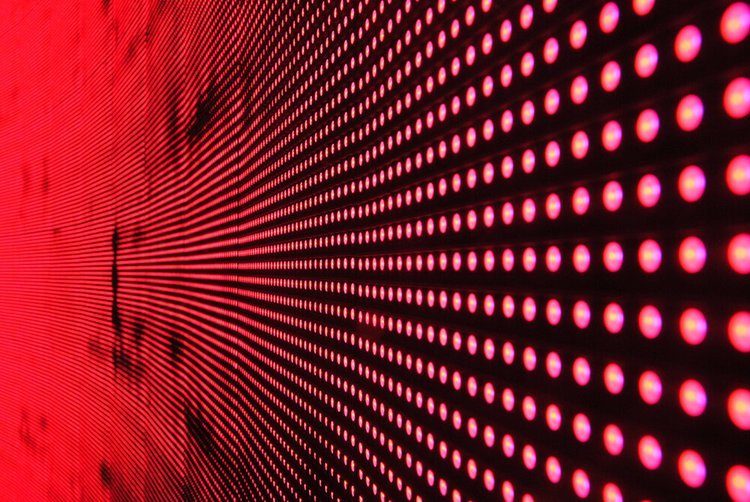
Glycemic variability (changes in blood sugar) are commonly present following TBI and can contribute to secondary brain injury and worse clinical outcomes. Continuous glucose monitors (CGMs) allow real-time, minimally invasive monitoring via a temporarily implanted sensor in the skin of the abdomen or arm. Several commercially available CGMs are used frequently for outpatients with diabetes, given their convenience, simplicity, and autonomous continuous collection of glucose readings (often every five minutes).
By applying CGMs to Emergency Department patients during the golden hours following TBI, the team aims to generate highly granular data of glycemic variability, and associate these findings with outcomes.
Development of an ultrasound-based flow-pressure index for the assessment of cerebral autoregulation
PI(s): J. Brian Fowlkes, PhD
After TBI, the vasculature can lose its ability to autoregulate blood flow to the brain. This loss of cerebral autoregulation (CA) is a major determinant of outcome after TBI. However, measuring CA is extremely difficult with the “gold standard” requiring placement of an intracranial pressure monitor as well as the need for continuous mean arterial pressure (MAP) monitoring.
The project team proposes to develop an alternative to PRx by replacing ICP as the measured variable with either internal carotid artery flow (ICA) or middle cerebral artery flow (MCA), combining one of these with MAP to develop a Flow-Pressure index (FPx) that is analogous to the invasive clinical standard.
Clinical development of LUCID: A therapeutic device for non-invasive mitochondrial modulation in adult TBI patients
PI(s): Florian Schmitzberger, MD, MS; Thomas H. Sanderson, PhD
Developing a neuroprotective approach for TBI is challenging due to differences in injury severity, location, and subtypes.
Mitochondrial dysfunction has been identified as a common component of TBI-induced cellular injury. Through their “LUCID” device, the project team has discovered novel effects of specific wavelengths of near infrared light (NIR) that allow modulation of mitochondrial activity. They aim to build on previous developments of LUCID, with the goal of testing it in optical phantoms and then in a clinical phase I trial on healthy human subjects.