Just Breathe: New Device Diagnoses Lung Diseases Using Exhaled Breath
JUST BREATHE: NEW DEVICE DIAGNOSES LUNG DISEASES USING EXHALED BREATH
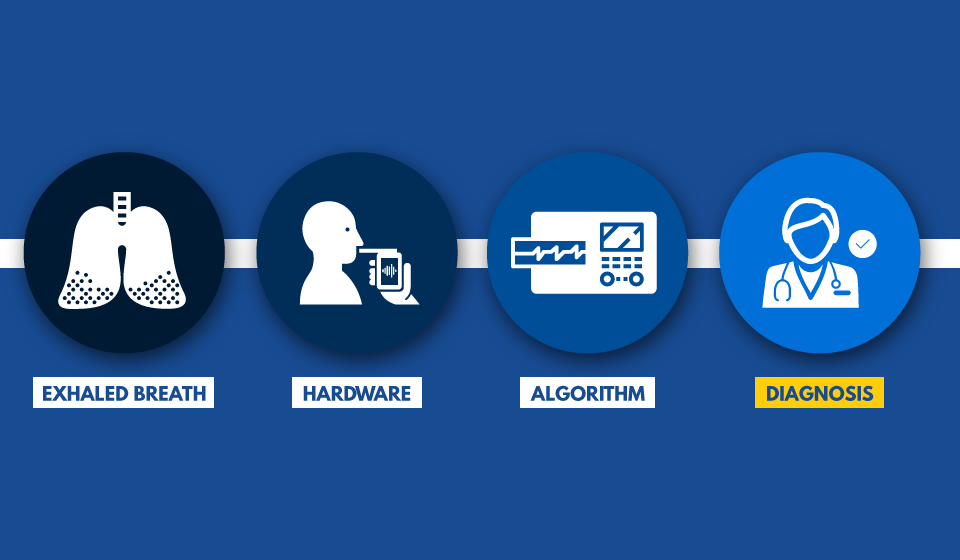
Breathalyzers have been used for decades to measure the amount of alcohol on breath, but what if they were able to detect illness? Researchers at the University of Michigan have developed a new point-of-care device that can diagnose life-threatening lung diseases using just a patient’s breath.
Exhaled breath contains hundreds of volatile organic compounds (VOCs) that carry important information about our physiology. Diseases can impact VOC combinations and create unique patterns known as a “breathomic signatures.”
Kevin Ward, MD, Executive Director of the Michigan Center for Integrative Research in Critical Care (MCIRCC) and Professor of Emergency Medicine and Biomedical Engineering, partnered with Xudong Fan, PhD, Associate MCIRCC Director and Professor of Biomedical Engineering, to develop a device that recognizes and analyzes breathomic signatures to help guide diagnosis.
While the technology, known as gas chromatography, has existed for years, the machines have never been practical for bedside monitoring. Ward and Fan have re-engineered this technology to analyze vapor molecules on a parts-per-billion scale.
“We’re able to get high-fidelity results in a much smaller package, and there’s no additional cost to the patient,” said Fan.
Currently, the researchers believe the device could help detect diseases such as Acute Respiratory Distress Syndrome (ARDS) days before a physician could make the diagnosis on their own. ARDS causes a buildup of fluid in the alveoli of the lungs, making it difficult for oxygen to reach other organs. The American Lung Association estimates 200,000 patients are diagnosed with ARDS each year. The disease is notoriously difficult to diagnose which is why it has such a high morbidity rate—between 30 and 50 percent die from the disease.
“ARDS is one of those diseases with a man-made definition. You can’t run a simple blood test or biopsy the lung, so it’s often tough to catch before it’s too late. Even conventional chest X-rays change late and can be difficult to interpret.” said Ward. Unlike biopsies or blood, breath can be collected non-invasively and continuously, making it an ideal sample.
Ward and Fan’s micro-gas chromatography device is fully automated and weighs only nine pounds. The device uses an algorithm that can generate diagnostic results in less than twenty minutes, so monitoring takes place in real-time. The device is also useful for monitoring patient trajectory once treatment has begun.
“Once you’re able to confirm the ARDS diagnosis and begin treating the patient, it can take a while to know if your treatment changes are working. This device enables a ‘breath by breath’ way to track progress, and you can know very early whether or not you’re going in the right direction,” said Ward. Additional team members include Dr. Robert Dickson, Assistant Professor of Internal Medicine and also an Associate Director for MCIRCC. Dr. Dickson is an expert in critical care and the role of the microbiome in ARDS and sepsis.
While treating ARDS is their main focus, both Ward and Fan envision this device improving outcomes for other inflammatory diseases such as pneumonia, sepsis, asthma and others. The team, initially funded by FFMI’s Michigan Translational and Commercialization program, has also received funding from the NIH’s Center for Accelerated Innovations based at the Cleveland Clinic. The data has been so promising (more than 90% accurate) that the team recently received an R21 exploratory/development grant from the National Institute of Health to advance the technology and test it in more patients. The team has several pending patents on the technology and is exploring starting a new company around the technology.
