Building an Ultrasound System to Detect Secondary Brain Injury
The reality of research is that many great ideas never move further than a casual chat with a colleague, or from the notes quickly scribbled down in the middle of the night. Research is costly and risky, and just having a brilliant idea is never enough.
But it is often those “risky” ideas that lead to transformational new technologies and treatments that could save lives. This is especially true for traumatic brain injury, where little advancement has been made in new treatments and technologies.
Each year, the Massey TBI Grand Challenge aims to provide an ecosystem where “risky” ideas can reach their fullest potential. Hosted by the Michigan Center for Integrative Research in Critical Care, the competition fosters interdisciplinary, milestone-driven research across devices, therapeutics, microfluidics, diagnostics, and health IT solutions.
The intensive process includes TBI education sessions, two rounds of proposal submissions, and project reviews by TBI experts from across the university, industry leaders, and the Department of Defense before teams receive funding. Once funded, the teams work closely with commercialization coaches to set milestones toward getting research from bench to the bedside.
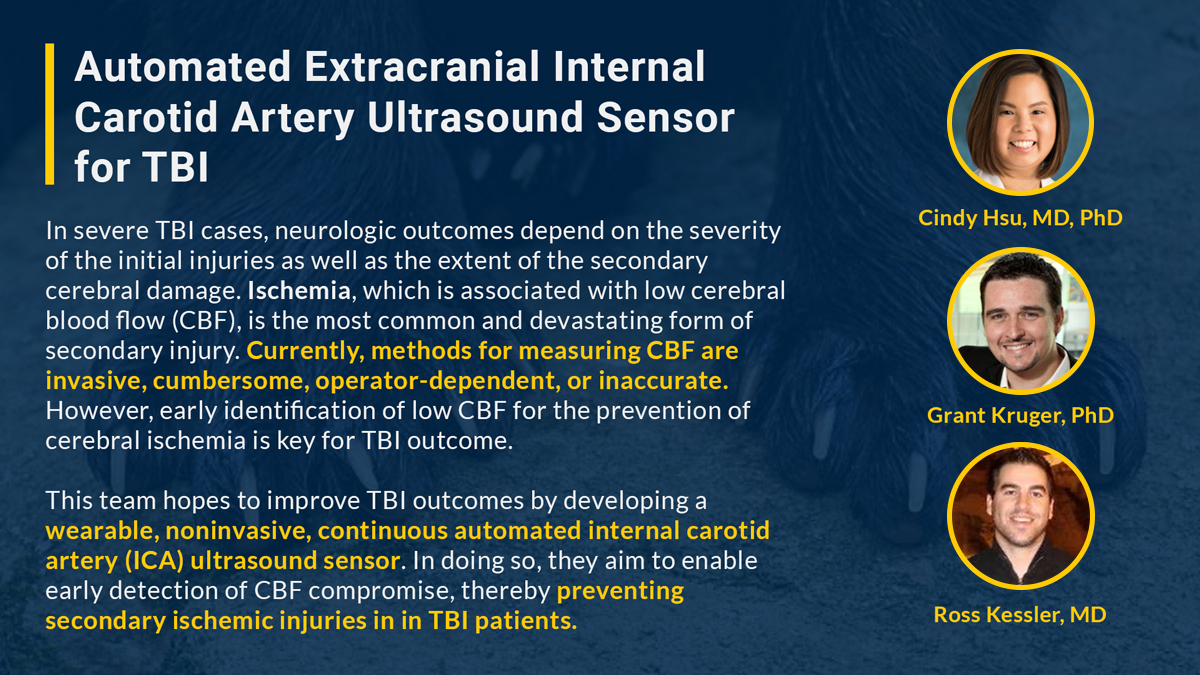
Last year, Grant Kruger, PhD, from the department of Mechanical Engineering, partnered with two Emergency Medicine physicians, Cindy Hsu, MD, PhD, and Ross Kessler, MD, to create an ultrasound system capable of detecting secondary brain injury. Their collaboration is an inspiring example of how engineering and medicine can come together to solve a difficult problem.
Coming from engineering, how did you start working on TBI research?
Kruger: Prior to coming to Michigan in 2007, my research focused on intelligent manufacturing systems. At that point I began investigating healthcare applications of my intelligent systems work by collaborating with various physicians. I now am fully engaged in the Smart Health research area, which investigates new technologies for collecting and analyzing patient data that assists clinicians in improving care.
I’ve always had a dream of improving the world in which we live. However, achieving this goal within healthcare requires teamwork. As a scientist and engineer, it is critical to work closely with physicians because they have real-world patient care experience. Not only do they understand the limitations of current care practices, but can also provide insight into the feasibility of integrating potential solutions within the care environment. While my research interest was never TBI specifically, this program provided a way for me to use technology I had already been working on in a new way that may have a real, positive impact to patient care and the potential to change the story of families like the Masseys.
How did you form your interdisciplinary team?
Hsu: Ross and Grant had been working on a different ultrasound sensor project through the Coulter Translational Research Partnership Program that was geared towards fluid management in sepsis patients. Ross, who is the Co-Director of Clinical Ultrasound, saw the potential for a similar sensor to be applied in TBI research when we discussed ways to non-invasively measure blood flow to the brain. When I met with Grant and Ross, we agreed there was a definite synergy between the two projects.
Can you tell us a little bit about your Grand Challenge project and how collaborating with an engineer has enabled a potential solution?
Hsu: Our common goal was to improve TBI care. We were looking for ways to prevent secondary injury and treat TBI patients more effectively. From the clinical perspective, we wanted to accurately detect compromise to cerebral blood flow (CBF). When CBF is compromised, it can lead to secondary brain injury and worse outcomes.
First, we brainstormed on how to non-invasively measure CBF using vessels in the neck. We know that we need to measure blood flow through the internal carotid artery (ICA). The ICA is challenging because of its proximity to other vessels in the neck and its gender and age-related variations across patients.
With Grant’s expertise in wearable sensor design and ultrasound algorithm development, we hope to build a sensor that can accurately locate the ICA and measure its flow non-invasively to detect changes in CBF.
Can you tell us about your experience working with someone from a different discipline on this project?
Kruger: Ross and Cindy have been a fantastic resource for discussing various concepts and requirements from a clinical perspective, and helping collect data to inform the algorithm development. When developing these kinds of technologies there is always a tradeoff between the clinical and engineering requirements and specifications, which can lead to some interesting and thought provoking discussions.
So far, the process has been somewhat technically intensive, but it’s really going get much more exciting when we start collecting data from human subjects using our prototype. That’s where we get to find out if all the clinical and engineering insight we’ve invested in the design has resulted in a prototype that is able to address the intended problem.
Hsu: Things that might seem intuitive to clinicians might not be intuitive for engineers, and vice versa. We speak different languages. For example, Grant asked us what would be the most important factors to consider when designing the shape of the ICA sensor. We knew that it needed to be extremely portable and stable so that it could fit on a patient’s neck during transport.
Then we had to consider that most TBI patients would be wearing a cervical spine collar for stabilization, so the sensor had to fit underneath that collar. When deciding on all of these design elements, we had to factor in the everyday challenges of the care providers. It’s been very helpful to break the problem down to make sure both sides understand the most important issues at hand.
What advice would you offer to other engineers looking to get involved with TBI research?
Kruger: From my experiences over the last 10 years at U-M, I have observed firsthand the fantastic environment within both the engineering and medical school for supporting this kind of research. Fundamentally, everyone shares a common passion for innovation and making a positive impact on society. The addition of their respective expertise provides a solid foundation for building excellent teams.
A unique feature of TBI treatment is that there are only a few acceptable options available to physicians that are currently available. Regardless of your scientific or engineering specialty, a huge scope exists for innovation—even small contributions can be rapidly translated and have the potential to save lives, improve quality of life, and minimize the impact of TBI on patients and their families. Physicians and patients urgently need these strong multi-disciplinary teams to develop improved treatment options to address the limitations of TBI care.
Do you have an idea that could improve TBI care? Attend the 2018 Massey TBI Grand Challenge on March 2 to hear from engineers, clinicians, patients, and more to find out how you can make a difference. Click here to register...
